- On-Call News
- Posts
- Stay or Repay? Mandatory NHS Service For Doctors
Stay or Repay? Mandatory NHS Service For Doctors
Would mandatory service post-medical school help with the NHS staffing crisis?
Contents (reading time: 7 minutes)
Stay or Repay? Mandatory NHS Service For Doctors
Weekly Prescription
Should Feelings Fund Care?
Board Round
Referrals
Weekly Poll
Stat Note
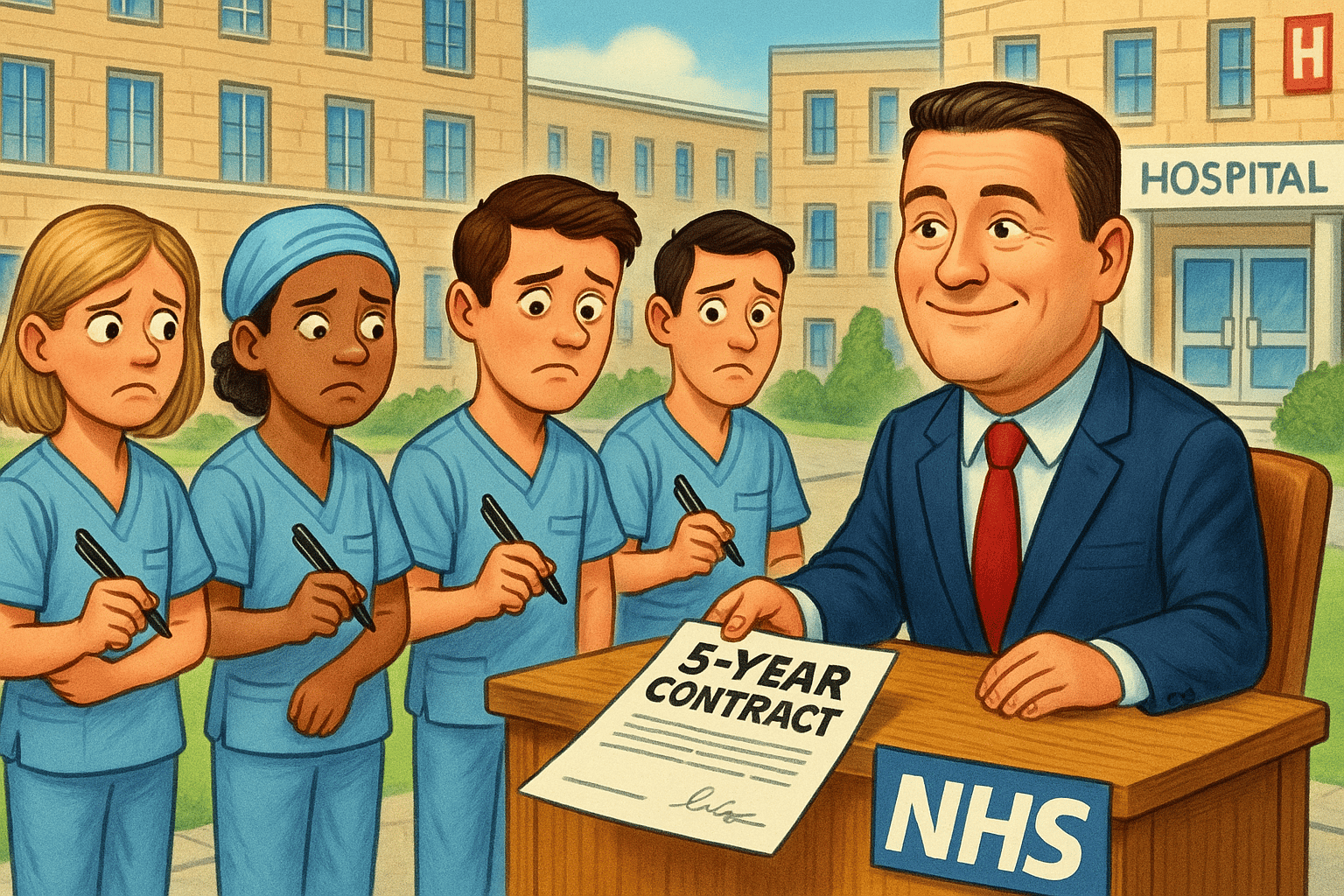
Stay or Repay?
Mandatory NHS Service For Doctors
Would mandatory service post-medical school help with the NHS staffing crisis?
You may remember the On-Call team saying in a previous article that any country that trains doctors only for them to leave once they reach the final stage of their careers is facing a crisis. This is undeniable.
It costs £230,000 to train a UK medical student - the majority of which comes from the taxpayer. The taxpayer also pays the salary of UK resident doctors. Resident doctors occupy training pathway spaces… and all this is perfectly okay because, eventually, our country gets amazing senior doctors and consultants, who act as our nation’s security blanket.
But this model relies on the UK actually retaining those doctors and with 18,000 UK trained doctors now practicing abroad, representing a 50% increase since 2008, something is clear - the NHS has a significant leak.
To maintain staffing levels, the UK has turned increasingly to international recruitment. Recent data shows that 60–65% of new NHS doctor registrations come from overseas-trained graduates. While these doctors are vital to service continuity, they are less likely to stay long term: only 10% remain in the UK after five years, compared to 75% of UK-trained doctors.
An NHS ‘Contract’
One proposed idea involves newly qualified doctors facing a period of mandatory NHS service after medical school. This is not purely academic, the idea was previously published in a 2017 document from the Department of Health titled Expansion of Undergraduate Medical Education. The length of this mandatory service has also been debated with no clear winner. Those who decide to leave early to work for a different organisation or to go oversees could be ordered to repay the funding invested in their education.
We see evidence of doctors undertaking mandatory service in the Armed Forces who also specify a period of minimum service, but unlike the Department of Health’s plans, the Armed Forces offer financial incentives including a generous bursary scheme and higher starting salaries on graduation.
It has become commonplace for doctors to take time out of training after completion of their foundation years and many of these doctors will venture to locations like Australia. Importantly however, most of these doctors return back to the UK.
It is unlikely that a period of mandatory NHS service will stop doctors from taking time out of the NHS to do additional years abroad once the mandatory service is complete, but it may increase the possibility that they may not return. Could it also lead to a shift in the attitudes of medical students who may begin preparing for USMLE and other international medical exams before the end of medical school?
You Don’t Own Me
The idea of the ‘social contract’ persists in Britain. Doctors were trained with public money, so the feeling they ‘owe’ the NHS is common place. But on economical grounds, compulsory service retains people and not necessarily their productivity. A demotivated and disengaged doctor in a pressured system will not deliver effective care.
Whilst it is difficult to argue with the concept economically, on an individual level it seems to somewhat contradict the modern liberal ideals of individual autonomy and the freedom of conscience. It reduces a human being and their agency to a type of debt instrument. Even if we dress this up in the language of ‘duty’, there is a prevailing message: the individual’s will is secondary to the state’s needs.
Now some may have no issue with the statement above, particularly in societies other than our own. It could be argued that autonomy does not exist within a vacuum and one’s ability to be a doctor is made possible by publicly funded universities and hospitals and state regulation. So this mandatory service would not be a ‘curtailment of freedom’, but the reality of inter-dependence that serves to keep the NHS on it’s feet by reducing staffing pressures.
Better Solutions?
Being sympathetic to the struggling economical situation of the state, perhaps the best solution lies in the middle ground. Like the armed forces who offer financial incentives for mandatory services, why could the government not look into tuition rebates where a portion of one’s loan is written off for 5 years NHS service?
Posts themselves should be of a sufficient quality for doctors to want to stay in the UK and the NHS. Being a doctor is conceptually a brilliant job and you should not have to tie doctors down to the NHS in order to keep them in the profession.
Perhaps instead we should be thinking about what it says about the NHS’s working standards and training opportunities, that mandatory service requirements are being considered to try to keep doctors here?

Would You Like Your NHS Receipt?
Britons don’t tire of mentioning that our health-service is free at the point of use. Many even wince at the thought of pay entering the healthcare conversation, but when it doesn’t, it is incredibly easy to forget how much the NHS spends. The media often quiz politicians on the price of a pint of milk to check they are in touch. Well here’s one for our On-Call community: How much does a CT Abdomen Pelvis cost the NHS?
One proposed solution has been to add the total cost of a patient’s care to their discharge letter. Not to shame, but to inform. When it became widespread to include calories on menus, there was inevitable push back from those who did not want to be reminded of such numbers.
But the reform went ahead, as the gain from having the information was seen as more important to the obesity crisis in the UK. Some make the same argument here - they claim knowledge is nearly always a good thing and will serve to promote shared responsibility and gratitude towards the NHS.
The risk here is the introduction of guilt and deterring people from seeking help who need it the most. Still, shielding the public from cost information isn’t sustainable. After all, patient’s aren’t just passive recipients of care, they are customers who fund the service through taxation.
Time to start thinking about your portfolio?
➡️ Need to develop your teaching skills?
➡️ Need to demonstrate your leadership capabilities?
➡️ Need to boost your portfolio ahead of interview season?
Perhaps Medset’s Train the Trainers and Leadership & Management courses might be the answers you were looking for…
Online and Live Virtual Classroom options available - use code ONCALL10 for a 10% discount.
Should Feelings Fund Care?
Is a patient-centred NHS ranking system the answer the government is looking for?

Many months ago, The On-Call team covered a proposal to introduce hospital rankings based on performance metrics like A&E waiting times. This time the NHS premier league table idea is back, but the headlines tell us that the government are planning to base it around a new metric - patient satisfaction.
It seems that under current plans, patients would be contacted a few weeks after their treatment with a simple question ‘Was your care good enough for the hospital to receive a full payment’. If the answer is no then around 10% of the standard rate will be diverted to a local improvement fund. The same article suggests maternity services will be the first to be targeted in this scheme, given the recent negative press they have received.
Healthcare is ultimately designed to serve our patients. We collate medical knowledge with the aim of making them healthier, and by extension, happier. This proposal however places patient satisfaction as the financial lever which introduces a whole new layer of complexity. But, as we noted in the last edition of On-Call news, our profession contains a unique ‘supplier-customer’ relationship.
In healthcare, patients are rarely in a position to judge whether their care ‘worked’ and they can’t easily critique what doctors know (well they certainly can critique, but with limited authority.) It’s a textbook case of information asymmetry.
Are All Complaints Equal?
Not all complaints or expression of dissatisfaction are created equally. A patient may be unhappy because they were not tended to appropriately (e.g it took 4 calls to raise a complaint to the nearest nurse) or because a symptom was missed by the medical team that later led to an apology. This type of complaint can be categorised as a service failure and can ubiquitously be agreed upon as it requires no esoteric medical knowledge to identify the error. Of course, in an ideal health system with no staffing or funding issues, it should not take you 4 calls to be tended to.
Another category of complaint however specifically concerns itself with clinical decisions: ‘The doctor wouldn’t give me morphine for my mechanical back pain’ and the issue is that patients are not in a position to discern the validity of their complaints if they pertain to medical practice.
In the age of the internet, patients arrive to medical encounters with preconceived expectations. They often make specific requests and recommendations to their doctors. Crucially, this sort of behaviour should not be immediately shut down. In fact we should want patients to be actively engaged with their health and pose questions to their doctors. The friction arises when clinical judgment clashes with patient demands.
The understanding patient will be eager to hear the doctors reasoning and have the intellectual maturity to trust that their knowledge of medicine is not as complete as the doctor sat across from them.
Patient satisfaction can not be the metric that we use to determine success. Take this paper published in JAMA which explored the relationship between patient satisfaction and health care use, overall expenditure, hospital stay and overall mortality. They found that higher patient satisfaction was associated with less emergency department use (fine), but greater inpatient use, higher overall healthcare and prescriptions and finally, increased mortality.
Patient experience is also determined by far more than their individual interaction with the clinician and so, unless this is very carefully designed and evaluated, there is a risk that providers could be penalised for more systemic issues. A two tier system could ensue with underfunded hospitals in deprived regions being further deprived of money due to poor survey results. This vicious feedback cycle seems to be a logical extension of the government’s new patient satisfaction scheme.

A round-up of what’s on doctors minds
“You can tell a lot from a doctor about their handover style. I am personally an over-seller, it may not sound much to you, but I can make any case sound like it needs your attention. Love my under-seller colleagues who can make the patient that has just arrested, had 3 rounds of CPR and IM adrenaline look like it’s nothing to get worked up over”
“I've just finished CT1 and no, I would not pick ACCS Anaesthetics again… I would pick core anaesthetics”
“Calculating pay deductions on strike day involves taking 1/365th of your annual salary for each striking day, or an hourly calculation rate that must be no greater than the 1/365th figure. This former tends to work out much less.”
“It’s 5pm and Nurse bleeps me asking for zopiclone because a patient can’t sleep. Not sure how others live their lives but I advised we should probably leave it til 10/11pm as nobody is meant to be sleeping at 5pm.”
What’s on your mind? Email us!

Some things to review when you’re off the ward…
This week, GP’s in England will be allowed to prescribe the weight loss jab, Mounjaro, but only under strict criteria such as having a BMI over 40 and four out of five key conditions.
If you are interested in public opinion of the BMA’s industrial action, a YouGov survey found that 36% of the public support further strike action whilst 49% oppose it. We can compare this to the last round where 59% of the public supported action vs 36% against.
Weekly Poll
How much does a CT Abdomen Pelvis cost the NHS? |
Last week’s poll:
Would you be comfortable being one of the NHS’s young consultants at 32 years old?

…and whilst you’re here, can we please take a quick history from you?
Something you’d like to know in our next poll? Let us know!

‘I’m Actually a Lawyer’: Defensive vs Reasonably Cautious Medicine
“And the next patient is a 54-year-old gentlemen presenting with abdominal discomfort and bloating on a background of Crohn’s disease. CT abdomen showed SBO with transition point at the terminal ileum… Oh and before we go in, he’s a solicitor and he will make sure you know”
Medical decisions are influenced by many factors, one of which is fear. Fear of uncertainty and the fear of being reprimanded which is only heightened with the mention of a patient with a legal background. This triggers our defensive response.
Numerous studies indicate that the more a doctor fears civil litigation, the more unnecessary tests they will order, in turn increasing the risk of false positives and further unnecessary and invasive procedures. Most people jump to extra tests when they think of defensive medicine, but the most common example is actually excessive documentation. Often the length and justification of a clinician’s documentation correlates with that doctor’s fear of litigation.
Ironically, most ‘I’m a lawyer’ patients are not even in medical negligence law, but for some, the phrase is enough to plant seeds of doubt. Seeds that create overcautious patterns and ultimately leaves doctors in this fatigue-inducing state of dissonance.
Most defensive practice actually takes place in the ‘grey areas’ of clinical judgement and in some cases, those extra ordered investigations could be interpreted as a doctor having a good degree of ‘reasonable caution’. So equally, it is vital we don’t create a narrative where ‘reasonable caution’ is conflated with lack of diagnostic skill or being ‘overly defensive’.
Help us build a community for doctors like you.
Subscribe & Share On-Call News with a friend or colleague!


Reply