- On-Call News
- Posts
- The UK Medical Training (Prioritisation) Bill Is Here Folks!
The UK Medical Training (Prioritisation) Bill Is Here Folks!
What this paradigm shift means for the NHS and its doctors
Contents (reading time: 7 minutes)
The UK Medical Training (Prioritisation) Bill Is Here Folks!
Weekly Prescription
Is the UKGP Bill Full of Holes?
Board Round
Referrals
Weekly Poll
Stat Note
A note from the editor…
Apologies that your inbox was deprived of last week’s edition of the newsletter. But thankfully we didn’t miss much… only the biggest shake-up in specialty training pathways for years!
We hope, as ever, that you enjoy this latest edition. On-Call News relies on you, the reader, to make this all worthwhile. So please keep reading, sharing and supporting news from those right on the frontline of healthcare with you.
The UK Medical Training (Prioritisation) Bill Is Here Folks!
What this paradigm shift means for the NHS and its doctors
On Tuesday, January 13, 2026, the government introduced the Medical Training (Prioritisation) Bill to the House of Commons in an attempt to address the systemic bottleneck currently locking thousands of UK medical graduates out of speciality training doors.
Since the 2022 policy shift that allowed international medical graduates (IMGs) to apply on equal terms with domestic candidates, we know that competition ratios have escalated to unprecedented levels. In justifying this legislative plan, Health Secretary Wes Streeting has invoked the principle of public investment, citing the £4.3 billion annual taxpayer contribution toward training medics as a mandate for domestic protectionism.
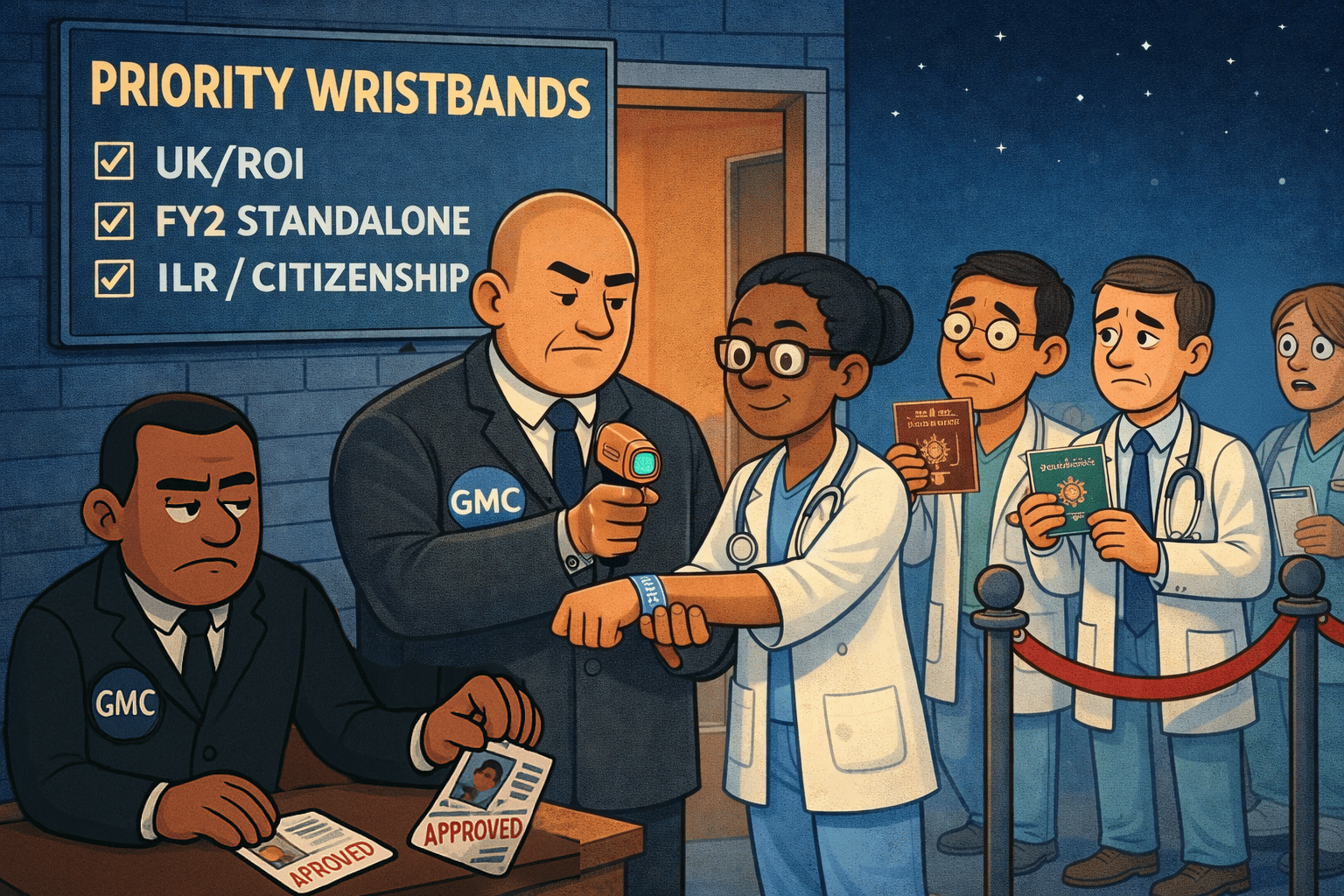
Who Is Front of The Queue?
The Bill does not merely favour UK graduates but establishes a tiered hierarchy that defines eligibility based on established criteria.
The main priority group are UK and Republic of Ireland medical graduates, alongside those from states such as Norway and Iceland due to existing reciprocal trade agreements. Another tier, often referred to as the NHS Continuity Group, includes doctors who have completed a UK Foundation Programme or an FY2 standalone year. This tier also extends to those holding British or Irish citizenship or Indefinite Leave to Remain. Doctors who have completed core training in the UK will also be prioritised. This means, for example, an IMG who has already completed Core Surgical Training in the UK and seeks an ST3 ENT post would remain eligible for prioritisation.
How Soon Are We Talking?
For the 2026 recruitment cycle, the government has proposed that this prioritisation will apply only at the offer stage. This is a critical distinction, as it means the government will not retrospectively review Internal Medicine Training (IMT) cases where candidates were unsuccessful in acquiring an interview.
However, from 2027 onwards, the prioritisation moves forward to the shortlisting stage, potentially preventing non-priority candidates from even reaching the interview phase. In order for the bill to become an act by the time offers are decided, the legislative timeline is moving quickly, with the second and third readings scheduled for January 26 and Royal Assent targeted for March 5. Given the cross-party support for the policy, the Bill is highly likely to pass through the House of Lords and into law without significant delay.
The Unlucky Losers
The human and legal costs of this transition are already making headlines. Many international medical graduates are facing substantial financial and professional upheaval as a result of these last-minute changes, particularly those who have passed the PLAB exams but have yet to secure NHS employment.
This mid-cycle implementation creates a clear legal vulnerability regarding unfairness and legitimate expectations, as many applicants structured their lives around the previous rules. While the courts cannot strike down primary legislation in the UK (as our politics textbooks tell us that our parliament is sovereign), a declaration of incompatibility with human rights remains a lingering threat to the government’s timeline.
Ultimately, the Bill represents a harsh return to the reality of state-funded education. While we sympathise with those excluded by these changes, the medical profession is no stranger to such upheaval. Just as medical students recently saw the value of their intercalated degrees and publications vanish overnight with the total restructuring of foundation school applications, this Bill asserts the state’s right to pivot its strategy during a jobs crisis.
When systemic change is pursued by the powers that be, the unfortunate reality is that one cohort’s stability often comes at the expense of another.

In the End Doctors, Who Do We Do This For?
It is impossible not to admire a doctor truly devoted to their craft. All of us at On-Call have, at some point in our careers, admired various doctors and surgeons who looked like they had it all together and reached a level of mastery in the profession. To reach this point, you have traded years for discipline and moments for exams. You have faced the relentless demands of clinical commitments and come out of the other end. Often, however, this has come at the direct expense of the people who love you most.
This is our On-Call plea for you to pause what you are doing on this Sunday morning (unless you are in the middle of something important, in which case, put your phone away).
In the quiet of a Tuesday morning, years from now, when your medical career is finally over, and you hit the snooze button, the hospital will continue to function. The rotas will be filled, the wards will remain busy, and the ticking machinery of the NHS will continue.
We need doctors who care deeply; medicine demands that level of soul-deep investment. No one can deny this. But we often forget a sobering truth: the NHS will eventually forget your late finishes, your skipped lunches, and your extra shifts. Your loved ones, however, will remember exactly how often you weren't there.
So, ask yourself, who are you doing this for?
Specialty Training Mock Interviews
Expert help from top performers
Give yourself the best chance of success with expert Courses and Mock Interviews, all delivered by previous top-performers who’ve aced their applications and interviews.
More than just practice scenarios, learn the frameworks that will allow you to maximise your performance and get the job you want.
CT/ST1 | ST3/4 |
Register for FREE interview prep webinars
Looking for Professional Development Courses?
Expert delivered training, on-demand, virtual classroom or in-person.
Is the UKGP Bill Full of Holes?
Why UK graduate prioritisation is a legal minefield
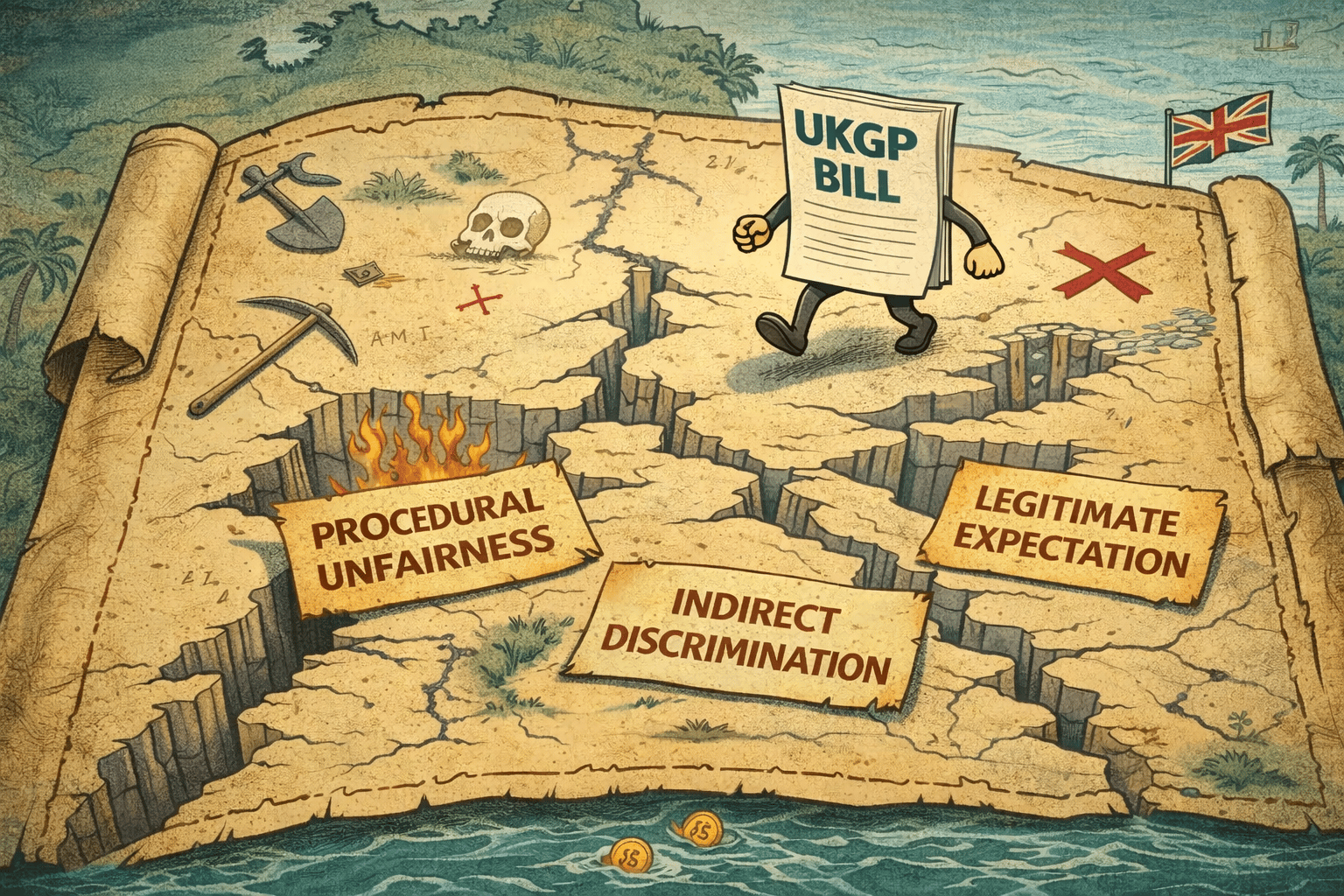
The On-Call team has been digging out their law textbooks, or rather, doing some aggressive research into the government’s new UK graduate prioritisation bill. We wanted to understand the specific "fault lines" where a legal challenge to the Medical Training (Prioritisation) Bill might actually hold some weight.
Here are some potential fault lines where a legal challenge could be mounted.
‘Mid-Cycle’ Unfairness
The most immediate challenge centres on Procedural Unfairness. The 2026 recruitment cycle is not just planned to happen; it is well and truly underway. Many International Medical Graduates (IMGs) have already incurred substantial "sunk costs," having sat the PLAB or MSRA exams and made life-altering logistical and financial commitments based on the published 2025/26 rules. Not to mention the emotional toll of ranking five equally bad SJT scenarios.
Parallels are already being drawn to the landmark BAPIO v Secretary of State case in 2008. In 2006, the Department of Health attempted to introduce a "Resident Labour Market Test" via guidance, which would have deprioritised international doctors in the middle of their careers.
The Supreme Court ultimately ruled that the government had acted unlawfully. They held that doctors who had been encouraged to come to the UK under specific work programs had a "legitimate expectation" that the rules of their employment and training wouldn't be rewritten by a mere departmental memo or ‘guidance’.
The Big Difference: Primary Legislation
However, there is a vital distinction between that landmark case and in 2026: this is not mere "guidance", it is Primary Legislation. In the UK’s system of Parliamentary Sovereignty, an Act of Parliament is significantly harder to overturn than a ministerial decision. While the 2008 BAPIO challenge succeeded because the government tried to bypass Parliament, the 2026 Bill is being pushed through the Commons and Lords with a deadline of March 5th for Royal Assent.
Because this is a Bill, the courts cannot simply "strike it down" for being unfair. Instead, any legal challenge would likely seek a Declaration of Incompatibility with the Human Rights Act. If a court finds that the Bill indirectly discriminates against IMGs without a "proportionate" justification, it doesn't invalidate the law, but it creates a massive political crisis and opens the door for significant compensation claims.
The government appears to be aware of its own vulnerability, however. By applying prioritisation only at the offer stage for 2026, and delaying the interview/shortlisting prioritisation until 2027, they are attempting a "soft launch" to mitigate claims of unfair discrimination.
The Verdict
So will the Bill survive its current form? We think so. With cross-party support and a fast-track timetable, the political momentum is simply too strong. The government’s strongest defence will be the ‘Objective justification’ that the sky-high competition ratios for UK graduates signal a workforce emergency that overrides individual expectations.

A round-up of what’s on doctors minds
“It’s not easy, especially on certain rotations, but try your best to do one thing at a time. There is no shame in telling people to speak to you later on. There is a significant underestimation in our profession of how cognitively damaging it can be to break a train of thought when you are in the middle of doing something. This is how bad outcomes happen.”
“Leeds, Birmingham, Shrewsbury and Telford Trusts are the three final trusts still using fax machines on a regular daily basis, according to our health secretary, who had no reservations publically naming and shaming them.”
“This week I broke new records of how many times as an ITU reg I needed to ask: 1) what the clinical question is for ITU? and 2) what ITU support the parent team is looking for?”
“Is it Feburary Yet?”
What’s on your mind? Email us!

Some things to review when you’re off the ward…
Resident doctors in England and Wales are keeping an eye on events over in Scotland, where the BMA has suspended pending strikes and put a new offer from the Scottish Government to voters. If accepted, it will give Scottish resident doctors an average uplift of 9.9% for 2025/26 and 9.4% for 2026/27. Read the full article here.
A new rule which urges doctors to ‘think again’ if they have been unable to reach a diagnosis after seeing a patient three times is to be advertised in all GP surgeries in England from next week. This new initiative, titled Jess’s Rule is named after Jessica Brady who contacted her GP on more than 20 occasions before she was eventually diagnosed with before her eventual cancer diagnosis.
Weekly Poll

Are you in favour of the BMA’s grandfathering policy, or does it defeat the purpose of the UK graduate prioritisation bill? |
Last week’s poll:
All other things being equal, would you be happy working a routine 80+ hour workweek in exchange for higher USA-levels of pay?

…and whilst you’re here, can we please take a quick history from you?
Something you’d like to know in our next poll? Let us know!

The Hospital Performance: It’s Okay To Not Be Infallible Doctors
"I’m not too certain about that one, Mrs Patel"
How often do those words feel like a professional failure? With the volume of medical literature doubling at a rate no human mind can match, missing a nuance is inevitable in medicine. Logic itself would therefore suggest that we should be comfortable expressing uncertainty.
Yet, the "theatre of medicine" rarely allows for it. We are conditioned to believe that reassurance is rooted in absolute knowledge. On the ward, there is a cultural expectation that a doctor must have every answer at hand. To admit doubt is often wrongly conflated with incompetence, and if we add the recognition that patients can rarely fact-check our claims, we create an environment filled with hyperbole, false confidence and sometimes, misinformation.
Is it any surprise, then, that we’ve created an environment where performance sometimes supersedes clinical accuracy? We’ve inadvertently selected for "authoritative, confident speech" as a key trait for career progression. While speaking with confidence is a skill, we must push against the creation of a culture which creates ‘good actors’.
Help us build a community for doctors like you.
Subscribe & Share On-Call News with a friend or colleague!


Reply