- On-Call News
- Posts
- The 22-Point Problem with IMT Applications
The 22-Point Problem with IMT Applications
With inflated portfolio requirements, is it even possible for F2s to progress directly into IMT anymore?
Contents (reading time: 7 minutes)
The 22-Point Problem with IMT Applications
Weekly Prescription
The Two-Year Life Span of The Trust-Grade Doctor
Board Round
Referrals
Weekly Poll
Stat Note
The 22-Point Problem with IMT Applications
With inflated portfolio requirements, is it even possible for F2s to progress directly into IMT anymore?

A couple of weeks have passed since we heard about the cut-offs for this year’s round of Internal Medical Training (IMT) applications. Budding physicians applied to IMT training based on the portfolio scoring matrix with the hope of securing that all-important interview. The portfolio contained requirements that we have come to expect of postgraduate applications (teaching, audits, publications and so on), but the recruitment process contained something new this year.
In an attempt to reduce applications and demonstrate a commitment to speciality, five extra points were awarded for those solely applying to IMT and nothing else. The cut-off was 22.
The Return of Dr. Al-Bumin
If we take Dr Al-Bumin, our hypothetical high-flying F2 who has made a unique application to IMT (5 points), has no postgraduate qualifications as they wished to progress straight from F2 (0 points), was keen during medical school and presented a cardiology poster at an international conference (4 points), published a case series on sick sinus syndrome as first author (3 points), got involved with regular teaching for over 3 months with feedback (3 points), managed to get the trust to cover a train the trainers course (1 point) and was involved in two cycles of a quality improvement project on CT angio scans (4 points).
Our F2 arrives at 20 points and falls just shy of the cut-off of 22 needed for an interview. Remove the unique application because of a fear of being without a job, and our F2 is in a dire situation.
What do you think of the above? We know many will see that portfolio and think it is stellar, but equally, some may disagree. They may believe that a portfolio with some teaching, presentations, audits and publications is almost mandatory, to be expected and should not be lauded as this amazing, unique achievement.
Whatever you think, one thing is for certain. In this climate, it has never been harder for our F2 colleagues to progress directly into training without beginning portfolio preparation earlier in their medical school years. Is this really what we want when students need to be learning the knowledge and skills they need to succeed in medicine and in wider life? The system is making it almost mandatory to add additional years to one’s training.
Message to our Medical Student Readers
To our medical student subscribers reading on, we know you are out there and perhaps worried about the direction our profession is moving towards. Sometimes in life, all one can do is react to the environment around them, with a recognition that the rules and paradigms could, and often do, change at any given moment.
We have always been practical here at On-Call and will continue to be so in our advice to you. Enjoy medical school, learn about the essence of medicine, and develop skills you will need in later life, such as good communication, confidence and a stoic attitude.
Make friendships, take time to see your family and pursue hobbies. But if you can, try your best to take steps towards building a portfolio early, as that will help you in later life.
You may be thinking, how on earth can I possibly know the speciality I am interested in at such an inexperienced age? A great point with no objective answer. Do not forget that for many, this idea of a speciality being your calling is a utopian fiction. Many people take their portfolio strengths, add a recognition of their personality traits (enjoys patient contact, likes a procedural speciality) and make an application.
Medical school is tough, but you often have access to leading academics and have the time to make mistakes. Trying to write up a manuscript or analyse a data set in between on calls can become incredibly challenging once you enter the workplace and that F2 application cycle comes around before you know it.
We know the climate may seem bleak for you. Remember that there is absolutely no shame in taking additional years after F2 to progress into training, especially when the system forces you into such a circumstance. Enjoy the journey, because it’s not a race.

This Christmas, the Media Will Be All Over Medics - Are the BMA Ready?
“The Medical Nightmare Before Christmas!”, “How the Doctors Stole Christmas!” or perhaps “Resident Doctor Strikes Create a Not-so-Silent Night!”
This round of strike action contains a unique element not seen in previous rounds of industrial action: the close proximity to Christmas. The timing is likely deliberate by the BMA, acknowledging the strain it will place on the NHS and the government during peak winter and flu season, while avoiding the danger of an understaffed ward in Christmas week, when many consultants intend to be with their families rather than covering for residents.
We know that, despite what we think on an individual level, humans are rarely rational actors. We use heuristics and biases to arrive at the conclusions we want rather than following the reasoning and seeing where it leads us. Tying this into the strike action, we know that the sentimentality surrounding Christmas will make this round of strikes incredibly unpopular with the public and the media, who will rely on any attempt to undermine the striking doctors.
We hope the BMA are ready with their best media-trained representatives. This barrage of LBC radio call-ins and Nick Robinson BBC interviews might be their toughest test yet.
Applying to Specialty Training?
Getting an interview can be hard enough – so once you’re there you need to give yourself the very best chance of success.
Medset’s expert Courses and Mock Interviews are delivered by previous top-performers who’ve aced their applications and interviews.
They’re more than just practice scenarios, you’ll learn the frameworks that will allow you to maximise your performance and get the job you want.
CT/ST1 | ST3/4 |
Need points for your specialty application?
Use our specialty application points calculator:
The Two-Year Life Span of The Trust-Grade Doctor
The hidden recommendation that keeps trust doctors on a two-year loop

If you work in a UK hospital long enough, you start spotting patterns: the empty staff car park on Fridays, the printer that never works, and of course, the mysterious two-year disappearance of the trust grade doctor.
Locally employed doctors (LEDs) are ever-growing and come with a variety of job titles: “clinical fellow,” “trust grade,” “trust-grade SHO,” “trust-grade registrar”, and the like. These contracts are attractive to trusts precisely because they allow enormous flexibility when it comes to pay, hours, teaching and supervision, all negotiable and often not in the doctor’s favour.
It is no secret that LEDs are the fastest expanding group in the medical workforce, and two-thirds of them qualified outside of the UK. The question not asked is this: why do these doctors almost never stay in the same trust in the same speciality for more than two years, even if they want to?
According to guidance from the Royal College of Physicians, if a doctor has been working in the same trust and the same speciality for more than two years, they should be moved onto a nationally negotiated contract. In other words, a proper specialist, associate specialist (SAS), or specialist doctor post, with real terms, protections and recognition.
But trusts know that a contractual upgrade shifts the power dynamic. Suddenly, the doctor gains defined pay scales, formal training expectations, job security and workplace rights. Meanwhile, the trust loses the flexibility that makes locally employed contracts so convenient in the first place.
So What Happens?
Doctors hit the two-year mark, and like clockwork, they are gently nudged and shepherded out of the post before the conversion can happen.
No conspiracies necessary, just a silent structural incentive built into the system. The result is an endlessly refreshed cohort of LEDs that never quite break through into stable roles.
It is an odd system indeed, where trusts get continuity without commitment, while LEDs get experience without security. And the NHS, which is increasingly reliant on internationally trained doctors, is having to deal with these questions on a more regular basis.
Any Answers, NHS Trusts?
For a trust, they may believe that given the sheer number of LEDs they employ, it is practically and fiscally unrealistic for all of them to be moved onto permanent contracts, and that doing so may detract from the training opportunities their trainees receive.
The argument could also be made that more checks and balances are needed to ensure the quality of a trust-grade doctor before they are appointed to a permanent post in the trust. To become a trainee, you go through national recruitment before being allocated a post, and as many doctors are trained abroad, it is difficult to assess quality without reviewing applicants on a case-by-case basis. Applying a blanket policy in which every doctor receives a permanent contract by virtue of two years of practice may be short-sighted.
Regardless, at least we now have an answer for the mystery of the two-year trust grade doctor.

A round-up of what’s on doctors minds
“Consultants refusing to cover shifts during the resident doctor strikes due to their proximity to Christmas could be a unique factor that separates this round of strike action from the previous 12 in recent times… Let’s wait and see.”
“I really think we are missing a trick in the narrative surrounding strike action. The jobs aspect of the industrial action and the suggested solutions are not being articulated anywhere near enough. All the media is writing about is pay.”
“My advice to all docs preparing for the FRCR is to nail key X-ray concepts as they are involved in CT, digital radiography, fluoroscopy, mammography, and radiation safety. I know the foreign nature of MRI may force you to over-prepare for it, but the MRI questions are few and far between. Good luck, especially when deciphering Farr’s.”
What’s on your mind? Email us!

Some things to review when you’re off the ward…
This article in the Financial Times shows the recent crisis our economy faces. Historically, it has been the elderly who have needed to take time off work due to ill-health and sickness. Today, we are facing a growing crisis of economically and socially displaced young adults. The share of young people who are not working, seeking work, not in education or raising children is approaching 10% in the UK and has doubled in the past decade.
The chair of the BMA, Dr Tom Dolphin, has become a familiar face representing the union in the media. Here he is in the Guardian fending off claims that he is weaponising the Resident doctor strikes by using them to progress his own political career after failing to be shortlisted as a Labour candidate in the 2024 general election.
Weekly Poll

Are you in favour of this next round of resident doctor strike action? |
Last week’s poll:
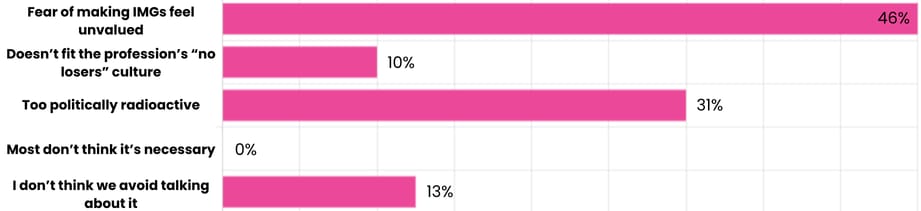
Why do you think doctors often avoid discussing UK graduate prioritisation?
…and whilst you’re here, can we please take a quick history from you?
Something you’d like to know in our next poll? Let us know!

For the Patient’s Sake, Just Do the Damn Clinical Exam
We often hear that technology and easy access to investigations are eroding clinical skills and thorough examination. Yes, we have written about this before (on multiple occasions). But have we considered all the consequences that the decline of clinical examination may have for our profession?
J. Tom Morgan, a family medicine doctor (or GP to you and me) at the Mayo Clinic, famously advised his interns: “Find a reason to examine the patient, even if it is only one or two systems. Nothing builds trust as quickly as a careful, competent exam where you make sure the patient is comfortable.”
Think about the public’s image of a doctor. Strip the profession down to its essence, and what comes to mind? Many would say the stethoscope. But the stethoscope is only a symbol. What it represents is the physical, hands-on act of examining a patient. This act is a type of performance. It demonstrates to the patient that we see and feel what they experience.
The clinical exam is what our profession has become associated with over the years, and there are perhaps few things as reassuring to our patients in knowing they are in the right hands than a thorough exam.
Help us build a community for doctors like you.
Subscribe & Share On-Call News with a friend or colleague!

Reply