- On-Call News
- Posts
- A House Divided: Why IMGs Hold The Key To The BMA’s Mandate
A House Divided: Why IMGs Hold The Key To The BMA’s Mandate
What the Ancient Greeks Can Teach the BMA about Democracy?
Contents (reading time: 7 minutes)
A House Divided: Why IMGs Hold The Key To The BMA’s Mandate
Weekly Prescription
The Quiet Capping of ADHD Assessments
Board Round
Referrals
Weekly Poll
Stat Note
A House Divided: Why IMGs Hold The Key To The BMA’s Mandate
What the Ancient Greeks Can Teach the BMA about Democracy?
As February 14th approaches, many of us find our phones buzzing more frequently with BMA notifications than with messages from potential romantic interests. There is a reason for this persistence: the BMA’s current mandate for industrial action is rapidly approaching its expiry date. To maintain its leverage, the BMA needs to ballot all resident doctors to extend that mandate.
The success of this movement hinges on a single metric: turnout. Under trade union law, if fewer than 50% of eligible members return their ballots, the mandate expires regardless of how many "Yes" votes are cast. This makes every demographic within the BMA, particularly the rapidly growing cohort of International Medical Graduates (IMGs), statistically vital for victory.
Vested Interests
However, a rift is appearing. On January 19th, Dr. Emma Runswick, Deputy Chair of the BMA Council, addressed a growing sentiment of boycott among IMGs on social media:
"IMGs - I’ve seen messages saying 'Don’t return your ballots' IGNORE THEM... Don’t help the government. Don’t wreck your chances to fight for pay and job."
The root of this tension lies in the Government’s recent "UK Graduate Prioritisation" legislation. Under these proposals, IMGs face an uphill struggle in training post applications, whilst UK graduates are prioritised. This is a legitimate grievance, and they will no doubt be the unlucky losers in this system. But as we have said previously, we invite someone to suggest a proposal that creates none of these unlucky losers. The government’s job in a democratic system is to reflect the will of the people, and wherever you fall on the UKGP divide, it is a policy that shares wide cross-party and public appeal.
The irony is that the BMA had long been lobbying for a two-year "grandfathering" clause to protect those already within the NHS, and it was likely that for IMGs the only protection they could seek was through the BMA. In a recent turn of events, however, official BMA outlets recently announced they would not be lobbying to change the government’s UKGP proposals.
Democracy and Its Paradoxes
We can learn a lot about democracy and its mechanics from this set of events. We are witnessing a shift in the "balance of power" within the union.
The Greek philosopher Plato served up one of democracy’s most significant critiques in The Republic, using the analogy of the Ship of State. If you were on a ship in a storm, would you want the captain to be selected by a popular vote of sailors who know little of navigation but are good at charming and rhetoric, or by the person who actually understands the stars and the wind?
There is much to be said about this, but there is a crucial insight we can take from Plato when looking at the BMA. Plato would argue that if a union’s policy is purely driven by what is popular amongst the loudest majority, it may ignore various truths and realities.
For many years, the BMA could focus on the concerns of UK graduates with little friction, as they represented the largest voting bloc. However, as the number of IMGs has grown significantly in the past couple of years, they have moved from a peripheral group to a significant deciding bloc. Many IMGs now acknowledge this power and the strength they have in unity. If the BMA ignores the specific existential threat facing IMGs, they risk a turnout failure. This is democracy’s ultimate check and balance: democratic leadership cannot ignore a significant minority.
How the BMA chooses to proceed is down to them; the success of their vote depends on it.

Is The “Referral Black Hole” Finally Closing?
For years, the concept of the NHS "referral black hole" has been a clinical nightmare. It is a void where tests and referral letters are either delayed, lost or not sent, leaving patients stranded in the dark. But new data suggests the black hole may be shrinking.
According to the latest Healthwatch England figures, one in seven patients now falls into this administrative hole, stuck waiting for letters that never arrive or appointments that weren’t booked. Whilst this number is significant, it is still a significant leap forward from 2023, when 21% or roughly one in five of patients were lost in the system.
Scary, isn’t it? To think you may be sitting on a significant pathology, waiting for tests or follow-ups that never happen. This is why we need to encourage patients to be advocates for their own health and to chase up things they feel they have been waiting on for too long. One in seven is, of course, still far too many, but at least we seem to be moving in the right direction.
Applying to Specialty Training?
Give yourself the best chance of success with expert Courses and Mock Interviews, all delivered by previous top-performers who’ve aced their applications and interviews.
More than just practice scenarios, learn the frameworks that will allow you to maximise your performance and get the job you want.
CT/ST1 | ST3/4 |
Looking for Professional Development Courses?
Expert delivered training, on-demand, virtual classroom or in-person.
The Quiet Capping of ADHD Assessments
Whilst GP’s are concentrating elsewhere, services for ADHD treatment are quietly being capped
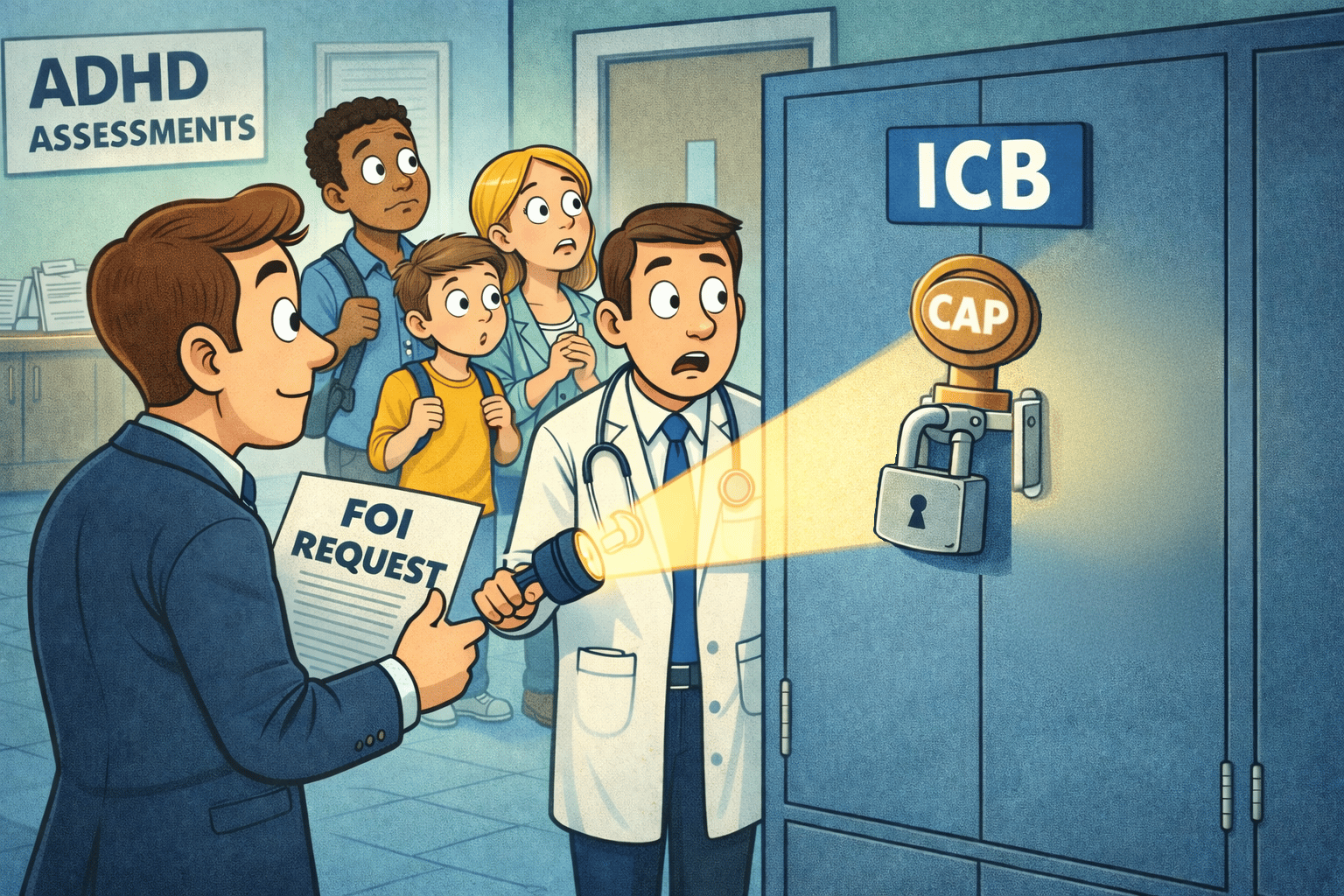
Savvy organisational operators all know the drill: if you want to do something unpopular, do it quietly. And that’s just the advice that NHS Integrated Care Boards (ICBs) have been following.
Last week, The Guardian reported that more than half of England’s ICBs have imposed limits on how many people can be assessed for ADHD, but what’s worse is that over half of these had not informed GPs or patients on the waiting list.
The information, obtained via a FOI request shows that despite soaring demand, services are being restricted in order save money. Now, as we’re said before, there is no magic money tree. However, the problem here lies in the lack of transparency.
This is rationing, which shouldn’t inherently be a bad word within a system with finite resources. But the problem is that we hate to acknowledge it. In a collective case of Orwellian double-think, we simultaneously, we know that there is only so much capacity in the system, yet we shudder when there is a restriction and some have to go without.
The cap that dares not speak its name
Instead of calling rationing what it is, we have other more harmless phrases like “capacity management” and “indicative activity”. However, these don’t really provide any comfort to the patient sitting across from you in your clinic room.
The reality is that ICBs are limiting assess to assessments for ADHD and autism. A waiting list is meant to be a crude promise: “We acknowledge the need; we cannot meet it yet; you will be seen in some order.” Once an unseen cap is applied, the waiting list becomes something else: an inbox where requests can accumulate without any meaningful relationship to delivery.
Why secrecy matters
Rationing exists in every healthcare system. But rationing without disclosure creates immediate, predictable harms. In this instance, it puts GPs in the firing line for a decision they did not make. And adding insult to injury, many of the ICBs had not informed GPs or patients. That’s not a minor admin oversight; it is a governance choice. Patients won’t blame an “indicative activity plan”. They will blame the person in front of them.
Secondly, it corrodes trust in the pathway. The public can tolerate “the NHS is under pressure”. What they struggle to tolerate is “the NHS is not being straight with you”.
What a grown-up response looks like
Step one of fixing this issue needs to be transparency. If a commissioner caps a funded activity, it should be visible to GPs and visible to patients. If the NHS believes a cap is ethically defensible, it should be defensible in the daylight.
Next, we need to stop treating waiting lists as passive objects. If waits are measured in years, “you’re on the list” is not really care. A waiting list should function as an active clinical register, with interim support, triage for risk, and escalation routes for deterioration.
Fundamentally, the NHS can be underfunded, overwhelmed, and still be honest. What it cannot afford is to become a system where access is shaped by hidden ceilings that clinicians only discover after patients have already spent months in limbo.

A round-up of what’s on doctors minds
“Did everyone know that 47% of 18 to 34-year-olds say that their car payment is as much as (or more than) their rent or mortgage. No wonder my car seems to be falling apart compared to most of the hospital car park.”
“There needs to be a strict tiering system for UKGP. UK graduates absolutely need to be placed in the top tier of preference, followed by IMGs who have served a certain number of years in the NHS.”
“My Friday evening task is sitting down with a glass of wine and picking apart my IMT interview in my head.”
“As an O&G reg, I’m not too certain on why most trusts still insist on pethidine for labour. The DIAMOND trial showed that for most metrics, morphine won, apart from the fact that it found that morphine/diamorphine did risk prolonging labour. But Pethidine is a worse analgesic, with a worse side effect profile and higher neonatal impact.
What’s on your mind? Email us!

Some things to review when you’re off the ward…
When it comes to hospital waiting lists, 31 hospital trusts have seen a decline, out of 129 trusts examined, according to the BBC. Here’s a useful tool by the BBC that shows how your nearest trust is doing.
Once upon a time, the advice was to get your exercise in. Nowadays, current research from Harvard School of Public Health tells us that variety is king. Those with the greatest variety of exercise had a 19% lower mortality risk compared to those who just focused on one activity. They also found the effect was greater with individual sports like jogging or tennis. Here’s a link to the full article.
Weekly Poll
Do you think capping ADHD assessment funding is fair? |
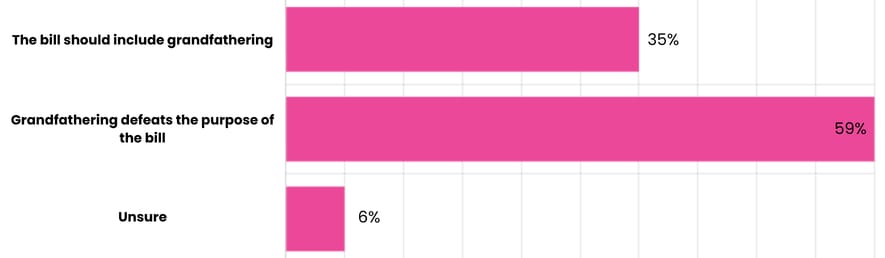
Last week’s poll:
Are you in favour of the BMA’s grandfathering policy, or does it defeat the purpose of the UK graduate prioritisation bill?
…and whilst you’re here, can we please take a quick history from you?
Something you’d like to know in our next poll? Let us know!

No ‘On-Call’ Doctor Should Go Anonymous Again
We’ve championed the "Hello, My Name Is..." campaign with our huge name badges and a movement to introduce ourselves to all patients, yet we remain remarkably comfortable being strangers to our colleagues. A formal introduction is something we are incredibly passionate about at On-Call, whether it be over the phone or in person.
When we bypass introductions, we fall into a bizarre "functionalist" trap, where we view our colleagues as mere occupiers of a role (the "Ward 14 nurse" or the "on-call SHO") rather than actual human beings with whom we should be collaborating. Observe any ward, and you’ll immediately see the friction that arises from anonymity.
This could be from a Consultant arriving at a new unit or a nurse managing a rotating bunch of resident doctors. Secondly, let’s not ignore the utilitarian thinking that suggests that clear role identification can offset the clinical risks associated with misattributed expertise. With all the best love in the world, a consultant cardiologist’s opinion on a NSTEMI is going to mean something different from an F2’s opinion.
You’ve earned your title through years of tough training. We promise you that using it is not an ego trip; it’s almost a prerequisite for working in a multidisciplinary fashion.
Help us build a community for doctors like you.
Subscribe & Share On-Call News with a friend or colleague!


Reply